For people 6+ with moderate to severe plaque psoriasis

IS THERE A CONNECTION BETWEEN MY PLAQUE PSORIASIS AND MY JOINT PAIN?
Are plaque psoriasis and psoriatic arthritis related?
Your skin and joints may have more in common than you think. The psoriasis plaques you see on your skin are believed to be the result of inflammation that may also lead to symptoms, like joint pain and swelling. Those symptoms are part of a connected disease, psoriatic arthritis, which can also lead to permanent joint damage, if left untreated. COSENTYX® (secukinumab) treats plaque psoriasis and psoriatic arthritis.
In a trial of patients with psoriatic arthritis, about 60% of patients taking COSENTYX 150 mg or 300 mg (versus 18% of patients taking placebo) saw at least a 20% improvement in psoriatic arthritis symptoms at 16 weeks.
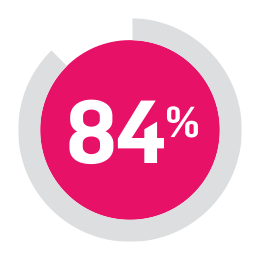
84% of people with psoriatic arthritis taking COSENTYX experienced no further joint damage at the 2 year mark.†
†About 76% of patients taking COSENTYX 150 mg or 300 mg had no further joint damage at the hands, wrists, and feet at Week 24, compared to 68% taking placebo. Everyone's experience is different. These results were from a less rigorous analysis, so it is not known if symptom improvement was due to COSENTYX. At 2 years, 84% of patients taking COSENTYX 300 mg had no further joint damage (71% of patients taking COSENTYX 150 mg).
THE PLAQUE PSORIASIS AND PSORIATIC ARTHRITIS CONNECTION
Watch this video to learn more about how both conditions could be connected.
Are you at risk for psoriatic arthritis?
Diagnosing psoriatic arthritis can be challenging because many of the symptoms are similar to those of other conditions. It can take many years for psoriatic arthritis to appear, so it's important to be aware of the connection to psoriasis.
What are some of the other risk factors for psoriatic arthritis aside from plaque psoriasis itself?
The severity of the plaque psoriasis—people with moderate to severe psoriasis carry a greater risk
Plaque psoriasis diagnosis at an earlier age
Having 3 or more sites on the body that are affected by plaque psoriasis
People with psoriasis who have lesions in their inner buttocks area are 2x more likely to develop psoriatic arthritis than those who don’t
3 or more visits to a dermatologist per year
Other skin and joint conditions
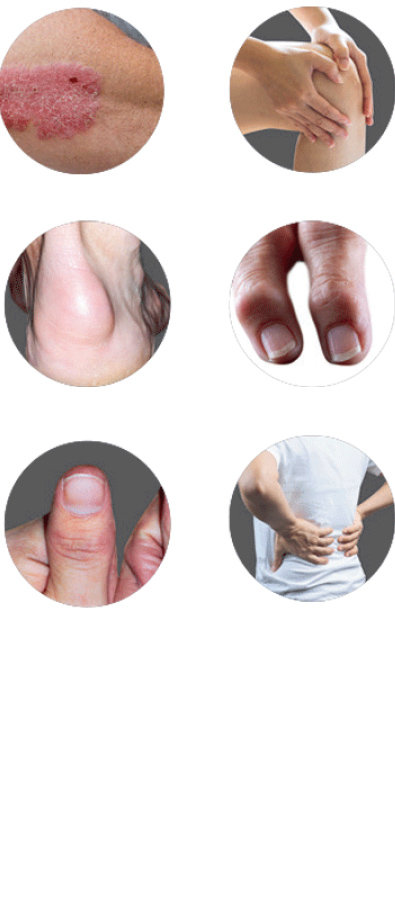
What are the symptoms of psoriatic arthritis?
Skin plaques and nail changes†: thick, red skin with flaky, silvery patches. Nail changes like separation from nail bed, pitting, or the appearance of a fungal infection
Joint pain and reduced range of motion: pain and swelling commonly felt in hands, feet, and joints
Tenderness in and around joints (enthesitis): pain or tenderness where tendons and ligaments attach to bones
Sausage-like fingers or toes (dactylitis): swelling along the entire length of finger(s) and toe(s)
Joint damage: if left untreated, psoriatic arthritis may cause permanent joint damage
Back pain (axial psoriatic arthritis), fatigue, and stiffness
About 85% of people with psoriatic arthritis experience plaque psoriasis symptoms first.
†Occurs in people who also have plaque psoriasis.
Take this quiz to find out if there’s more to your psoriasis
It’s not always easy to explain how you feel. Taking this quiz could help. If you answered yes to 3 or more of these questions, make sure to talk to your doctor at your next appointment about plaque psoriasis and psoriatic arthritis. It’s important to talk to your doctor as soon as you can. A delay in diagnosis of psoriatic arthritis by as little as 6 months can lead to permanent joint damage.
1. Have you ever had a swollen joint (or joints)?
2. Has a doctor ever told you that you have arthritis?
3. Do your fingernails or toenails have holes or pits?
4. Have you had pain in your heels?
5. Have you had a finger or toe that was completely swollen and painful for no apparent reason?
This tool is the PEST (Psoriasis Epidemiology Screening Tool) questionnaire developed by GH Ibrahim et al.
Is family history a risk factor for psoriatic arthritis?
Family history can be a risk factor for psoriatic arthritis. If any of your close relatives have plaque psoriasis or psoriatic arthritis, you could have a greater chance of getting either or both conditions.
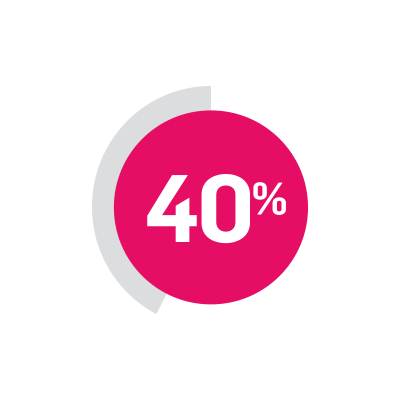
40% of people with psoriatic arthritis have at least one close relative with psoriatic arthritis or psoriasis.

Make your next appointment count.
Our doctor conversation starter can help you document your PsO symptoms, in one place, so you’ll feel more prepared for future appointments.
Real people have found real relief from both conditions with COSENTYX.
See how COSENTYX helps relieve symptoms of plaque psoriasis and psoriatic arthritis.
